Description
Cefepime: A Comprehensive Overview
Cefepime, a fourth-generation cephalosporin antibiotic, is widely utilized for its broad-spectrum activity against a range of Gram-positive and Gram-negative bacteria. Approved by the U.S. Food and Drug Administration (FDA) in 1996, it is recognized for its effectiveness in treating various severe infections, particularly in hospital settings.
Mechanism of Action
Cefepime works by interfering with the synthesis of bacterial cell walls. It binds to penicillin-binding proteins (PBPs) located in the bacterial cell membrane, inhibiting the transpeptidation process, which is essential for cell wall formation. This action causes the bacteria to be unable to maintain their structural integrity, leading to cell lysis and ultimately bacterial death. With its capability to penetrate the outer membranes of Gram-negative bacteria, cefepime demonstrates increased activity against organisms that are typically resistant to older antibiotics.
Spectrum of Activity
Cefepime exhibits a broad spectrum of activity:
- Gram-positive bacteria: This includes Streptococcus pneumoniae and Staphylococcus aureus (methicillin-susceptible stains).
- Gram-negative bacteria: Cefepime is particularly effective against Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and various Enterobacter species.
Due to its enhanced stability against many beta-lactamases—enzymes produced by bacteria that confer resistance to beta-lactam antibiotics—cefepime is often a go-to choice for treating infections caused by resistant strains.
Indications
Cefepime is indicated for the treatment of several serious infections, including but not limited to:
- Pneumonia: Particularly in hospital-acquired or ventilator-associated cases.
- Urinary Tract Infections (UTIs): Effective against complicated UTIs caused by susceptible organisms.
- Skin and Soft Tissue Infections: Including those caused by different strains of staphylococci and streptococci.
- Intra-Abdominal Infections: Particularly in severe cases that may necessitate combination therapy.
Additionally, it is commonly employed as part of empirical therapy for febrile neutropenia, often in combination with other agents.
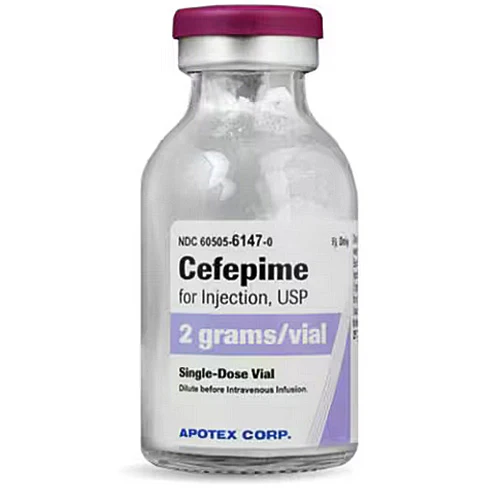
Administration and Dosage
Cefepime is administered intravenously or intramuscularly, with dosages typically tailored based on the severity of the infection, the patient’s renal function, and the pathogen’s susceptibility. The standard adult dosage for most indications ranges from 1 to 2 grams every 8 to 12 hours, with adjustments made for patients with renal impairment.
Side Effects and Precautions
As with any antibiotic, cefepime can cause a range of side effects. Common adverse reactions include:
- Gastrointestinal disturbances: Such as nausea, vomiting, and diarrhea.
- Hypersensitivity reactions: Ranging from mild rashes to severe anaphylactic reactions.
- Hematologic changes: Including leukopenia, neutropenia, and thrombocytopenia.
- Neurological effects: High doses or rapid infusion may result in neurotoxicity, leading to seizures or encephalopathy.
Due to these potential side effects, monitoring for both renal function and any adverse reactions is critical during therapy. Additionally, a thorough medical history should be obtained to assess previous allergies or reactions to beta-lactam antibiotics.
Emerging Resistance and Future Considerations
As bacterial resistance continues to evolve, the efficacy of cefepime and similar antibiotics can be compromised. Resistance mechanisms such as the production of extended-spectrum beta-lactamases (ESBLs) and other modifying enzymes are growing concerns. Consequently, the development of combination therapies and new agents is necessary to address the challenge of resistant infections.
Conclusion
Cefepime remains an essential antibiotic in modern medicine, particularly in treating serious infections in hospitalized patients. Its broad spectrum, effective penetration against Gram-negative bacteria, and stable performance against beta-lactamases make it a valuable asset in the antibiotic arsenal. As resistance patterns shift, ongoing surveillance and prudent use of cefepime are vital to preserve its effectiveness and ensure optimal patient outcomes.














Reviews
There are no reviews yet.